Cataracts
Highlights
Cataracts
Cataracts are a common age-related vision problem. About 22 million Americans age 40 and older have cataracts, and the older a person gets the greater the risk for developing cataracts. Women are more likely to develop cataracts than men, and African-Americans and Hispanic Americans are at particularly high risk.
In addition to age, other factors may increase the risk of cataract development. These include:
- Diabetes
- Smoking
- Overexposure to sunlight
- Certain medications, such as steroids
Symptoms
During the early stages, cataracts may have little effect on vision. Symptoms vary due to the location of the cataract in the eye (nuclear, cortical, or posterior subcapsular). Depending on the type and extent of the cataract, patients may experience the following symptoms:
- Cloudy vision
- Double or blurry vision
- Glare and sensitivity to bright lights
- Colors appear faded
- Difficulty reading due to reduced black-white contrast
- Difficulty driving at night
Treatment
Cataracts never go away on their own, but some stop progressing after a certain point. But if cataracts continue to grow and progress, they can cause blindness if left untreated. Fortunately, cataracts can almost always be successfully treated with surgery. Millions of cataract operations are performed each year in the United States, and there is a very low risk for complications. However, before opting for surgery, patients need to consider on an individual basis how severely a cataract interferes with their quality of life. Cataract surgery is rarely an emergency, so patients have time to consult with their doctors and carefully consider the risks and benefits of surgery.
Cataract Removal Surgery
Surgery involves removing the cataract and replacing the abnormal lens with a permanent implant called an intraocular lens (IOL). The operation takes less than 1 hour and is performed on an outpatient basis. The procedure is generally painless and most patients remain awake, but sedated, during it. If you have cataracts in both eyes, doctors recommend waiting at least 1 month between surgeries.
Introduction
A cataract is an opacity, or clouding, of the lens of the eye.
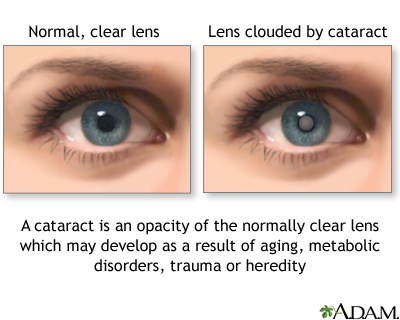
The likelihood of developing cataracts increases with age. Cataracts typically occur in the following way:
- The lens is an elliptical structure that sits behind the pupil and is normally transparent. The function of the lens is to focus light rays into images on the retina (the light-sensitive tissue at the back of the eye).
- In young people, the lens is elastic and changes shape easily, allowing the eyes to focus clearly on both near and distant objects.
- As people reach their mid-40s, biochemical changes occur in the proteins within the lens, causing them to harden and lose elasticity. This causes a number of vision problems. For example, loss of elasticity causes presbyopia, or far-sightedness, requiring reading glasses in almost everyone as they age.
- In some people, the proteins in the lens, notably those called alpha crystallins, may clump together, forming cloudy (opaque) areas called cataracts. They usually develop slowly over several years and are related to aging. In some cases, depending on the cause of the cataracts, loss of vision progresses rapidly.
- Depending on how dense they are and where they are located, cataracts can block the passage of light through the lens and interfere with the formation of images on the retina, causing vision to become cloudy.
Cataracts can form in any of three parts of the lens and are named by their location.
- Nuclear cataracts. These form in the nucleus (the inner core) of the lens. This is the most common type of cataract associated with the aging process.
- Cortical cataracts. These form in the cortex (the outer section of the lens).
- Posterior subcapsular cataracts. These form toward the back of a cellophane-like capsule that surrounds the lens. They are more frequent in people with diabetes, those who are overweight, or those taking steroids.
Causes
Although older age is the primary risk factor for cataracts, researchers are still not certain about the exact biologic mechanisms that tie cataracts to aging.
Oxygen-Free Radicals (Oxidants) and Glutathione
Particles called oxygen-free radicals may be a major factor in the development of cataracts. They cause harm in the following way:
- Oxygen-free radicals (also called oxidants) are molecules produced by natural chemical processes in the body. Toxins, smoking, ultraviolet radiation, infections, and many other factors can create reactions that produce excessive amounts of oxygen-free radicals. When oxidants are overproduced, these chemicals can be very harmful to cells throughout the body.
- Cataract formation is one of many damaging changes that can occur from overproduction of oxidants, possibly in combination with deficiencies of an important protective anti-oxidant called glutathione.
- Glutathione occurs in high levels in the eye and helps fight back against free radicals. One theory is that in the aging eye, barriers develop that prevent glutathione and other protective antioxidants from reaching the nucleus in the lens, thus making it vulnerable to oxidation.
Radiation and Electromagnetic Waves
Sunlight and Ultraviolet Radiation. Sunlight consists of ultraviolet (referred to as UVA or UVB) radiation, which penetrates the layers of the skin. Both UVA and UVB have damaging properties that can promote cataracts. The eyes are protected from the sun by eyelids and the structure of the face (overhanging brows, prominent cheekbones, and the nose). Long-term exposure to sunlight, however, can overcome these defenses.
- UVB radiation produces the shorter wavelength, and primarily affects the outer skin layers. It is the main cause of sunburn. It is also the type of UV radiation primarily responsible for cataracts. Long-term exposure to even low levels of UVB radiation can eventually cause changes in the lens, including pigment changes, which contribute to cataract development. (UVB also appears to play a role in macular degeneration, an age-related disorder of the retina.) Some scientists suggest that global warming and ozone depletion may increase people’s exposure to UVB, leading to a greater incidence of cataracts.
- UVA radiation is composed of longer wavelengths. They penetrate more deeply and efficiently into the inner skin layers and are responsible for tanning. The main damaging effect of UVA appears to be the promotion of the release of oxidants.
Radiation Treatments. Cataracts are common side effects of total body radiation treatments, which are administered for certain cancers.
Electromagnetic Waves. Questions have been raised about the hazards of low-level radiation from computer screens. To date, no study has demonstrated an association between cataract development and video display terminals. It is a good idea, in any case, to sit at least a foot away from the front of a screen.
Medications
Corticosteroids. Long-term use of oral steroids is a well-known cause of cataracts. Studies have been conflicting, however, over whether inhaled and nasal-spray steroids increase the risk for cataracts. Information on cataract risk from inhaled steroids is important because they are commonly used for treatment of asthma and allergies.
Other Medications Associated with Cataracts.
- Psoralens, a class of drugs used along with light therapy to treat skin disorders, such as psoriasis
- Antipsychotic medications such as chlorpromazine (Thorazine)
- Glaucoma medications
Many others drugs have been weakly associated with cataracts, including allopurinol, tamoxifen, amiodarone, tricyclic antidepressants, potassium-sparing diuretics (but not other diuretics), thyroid hormone, tetracyclines, sulfamidase, and mepacrine. Statin drugs (used for managing cholesterol) may possibly reduce the risk for nuclear cataracts.
Causes of Cataracts in Children
Rarely, about 1 in every 10,000 births, a baby is born with cataracts (called congenital cataracts).
- Inherited disorders are often involved in the development of congenital cataracts in children. Such cataracts are most often due to inborn abnormalities in the structure or shape of the lens, including its capsule. Certain types of genetic factors may play a role.
- Infection during pregnancy can lead to cataracts.
- Pregnant women who abuse alcohol or drugs increase the risk for cataracts (along with other more serious birth defects) in their infants.
Risk Factors
Aging is the primary risk factor for cataracts, but other factors are also involved.
Age
Nearly everyone who lives long enough will develop cataracts to some extent. Some people develop cataracts during their middle-aged years (40s and 50s), but these cataracts tend to be very small. It is after age 60 that cataracts are most likely to affect vision. Nearly half of people age 75 and older have cataracts.
Gender
Women face a higher risk than men.
Family History
Cataracts tend to run in families.
Race and Ethnicity
African-Americans have nearly twice the risk of developing cataracts as Caucasians. This difference may be because African-Americans are also more likely to have diabetes, which is a risk factor for cataracts. African-Americans are much more likely to become blind from cataracts and glaucoma than Caucasians, mostly due to lack of medical care.
Hispanic Americans are also at increased risk for cataracts. In fact, cataracts are the leading cause of visual impairment among Hispanics.
Glaucoma and Other Eye Conditions
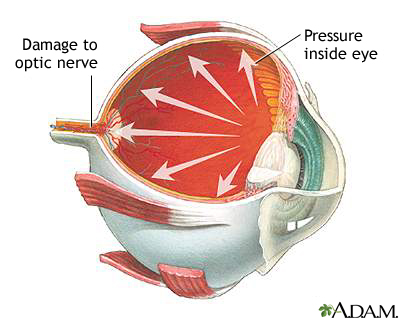
Glaucoma. Glaucoma and its treatments, including certain drugs (notably miotics) and filtering surgery, pose a high risk for cataracts. The glaucoma drugs that can increase risk for cataracts include demecarium (Humorsol), isoflurophate (Floropryl), and echothiophate (Phospholine).
Myopia. People who are nearsighted (myopic) are at increased risk of developing cataracts.
Uveitis. Uveitis is chronic inflammation in the eye, which is often caused by an autoimmune disease or response. Often the cause is unknown. It is a rare condition that carries a high risk for cataracts.
Other Eye Conditions. Physical injuries to the eye (such as a hard blow, cut, or puncture) or eye inflammation can also increase risk. Previous intraocular eye surgery increases cataract risk.
Other Medical Conditions
Diabetes. People with diabetes type 1 or 2 are at very high risk for cataracts and are much more likely to develop them at a younger age. They also have a higher risk for nuclear cataracts than nondiabetics. Cataract development is significantly related to high levels of blood sugar (hyperglycemia). Obesity, which is associated with diabetes type 2, may also be a risk factor for cataracts.
Autoimmune Diseases and Conditions Requiring Steroid Use. Medical conditions requiring long-term use of oral corticosteroids (commonly called steroids) pose a particularly high risk. Many of these medical conditions are autoimmune diseases, including rheumatoid arthritis, psoriasis, multiple sclerosis, systemic lupus erythematosus, Behcet's disease, and others.
Overexposure to Sunlight
Exposure to even low-level UVB radiation from sunlight increases the risk for cataracts, especially nuclear cataracts. The risk may be highest among those who have significant sun exposure at a young age. People whose jobs expose them to sunlight for prolonged periods are also at increased risk.
Smoking and Alcohol Use
Smoking. Smoking a pack a day of cigarettes doubles the risk of developing cataracts. Smokers are at particular risk for cataracts located in the nuclear portion of the lens, which limit vision more severely than cataracts in other sites.
Alcohol. Chronic heavy drinkers are at high risk for a number of eye disorders, including cataracts.
Environmental Factors
Long-term environmental lead exposure may increase the risk of developing cataracts. Gold and copper accumulation may also cause cataracts. Prolonged exposure to ionizing radiation (such as x-rays) can increase cataract risk.
Prognosis
Some cataracts stop progressing after a certain point but they never go away on their own. If extensive and progressive cataracts are left untreated they can cause blindness. In fact, cataracts are the leading cause of blindness among adults age 55 and older.
Fortunately, cataracts can nearly always be successfully removed with surgery. However, surgery is unavailable in certain parts of the world, leaving millions at risk for vision loss. Even in the U.S., where surgery has greatly reduced the risk of blindness, tens of thousands still lose their sight and millions more have poor vision because of cataracts.
Effect on Daily Functioning
Some people who have small cataracts can see well enough around the clouded areas to live normally. Extensive cataracts, however, can affect people’s abilities to earn a living, read, drive, or live independently and can interfere greatly with daily activities.
Prevention
Although cataracts are not completely preventable, their occurrence can be delayed. Quitting smoking, avoiding overexposure to sunlight, avoiding excessive amounts of alcohol, and eating plenty of fresh fruits and vegetables are important protective measures. There is no proof that using eye drops or ointments or performing eye exercises can prevent the onset of cataracts.
Avoiding Ultraviolet Radiation
The simplest and most effective way to protect against ultraviolet (UV) radiation is to stay out of the sun. Wear a hat and cover-up outside, especially when the sun is most intense (10 a.m. - 3 p.m.). A wide-brimmed hat can significantly reduce eye exposure to UVB radiation. Because the sun's rays are highly reflective, sitting in the shade or under an umbrella by itself does not guarantee protection.

Note: Moderate sun exposure provides an important source of vitamin D, which is essential for healthy bones and other health factors. Fortunately, people who protect themselves from the ultraviolet radiation in sunlight can get the vitamins they need from supplements.
Sunglasses. Protective sunglasses do not have to be expensive. But it is important to select sunglasses whose product labels state they block at least 99 percent of UVB rays and 95 percent of UVA rays.
Polarized and mirror-coated lenses do not offer any protection against UV radiation. It is not clear if blue light-blocking lenses, which are usually amber in color, provide UV protection.
Diet and Nutrition
Scientists are not certain if nutrition plays a significant role in cataract development. Dark colored (green, red, purple, and yellow) fruits and vegetables usually have high levels of important plant chemicals (phytochemicals) and may be associated with a lower risk for cataracts.
In analyzing nutrients, researchers have focused on antioxidants and carotenids. Studies have not demonstrated that antioxidant vitamin supplements (such as vitamins C and E) help prevent cataracts. Still, fruits and vegetables containing these vitamins are important for overall good health.
Lutein and zeaxanthin are the two carotenids that have been most studied for cataract prevention. They are xanthophylis compounds, which are a particular type of carotenid. Lutein and zeaxanthin are found in the lenses of the eyes. Some evidence indicates that xanthophyll-rich foods (such as dark green leafy vegetables) may help slow the aging process in the eye and protect against cataracts. However, there is not enough evidence to suggest that taking supplements that contain these carotenoids lowers the risk for cataract formation.
Symptoms
During the early stages, cataracts have little effect on vision. As the cataract progresses, symptoms may include:
- Cloudy vision, double vision, or both may be the first signs.
- Images may take on a yellowish tint as color vibrancy diminishes.
- Reading may become difficult over time because of a reduced contrast between letters and their background.
- Sensitivity to bright lights may make it difficult or impossible to drive at night because of glare from the headlights of oncoming cars. (People with diffuse cataracts in the rear walls of their lenses are particularly prone to glare sensitivity because bright light tends to scatter in their lenses.)
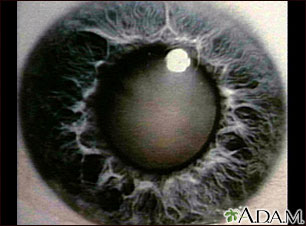
- In very advanced cases, the pupil, which is normally black, looks milky or yellowish. The patient's vision is reduced to being able only to distinguish light from dark.
Symptoms may vary depending on the part of the lens that is affected.
Nuclear Cataracts. Cataracts of the lens nucleus are most commonly associated with aging. Symptoms include:
- Hazy distance vision and increasing glare.
- Progressive nearsightedness and the need for frequent changes in eyeglass prescriptions. This effect may even temporarily counteract age-related farsightedness and provide a temporary improvement in overall vision in some people. The improvement fades when the cataract advances sufficiently to overwhelm the inherent farsightedness. Eventually, as the cataract grows worse, stronger glasses can no longer correct the patient's vision.
Cortical Cataracts. Cortical cataracts usually start on the outside of the cortex (the outer area of the lens).
- They have very little initial effect on vision.
- Glare can develop as these cataracts increase and approach the center of the lens.
- Problems with distance vision, contrast sensitivity, and clarity may occur as the cataracts progress further.
Posterior Subcapsular Cataracts. Posterior subcapsular cataracts typically start near the center of the back part of the capsule surrounding the lens. These cataracts often advance rapidly. For many patients, major impairment of eyesight, including near-vision problems and glare, develops within several months.
Diagnosis
Either an ophthalmologist or an optometrist can examine patients for cataracts, but only ophthalmologists are qualified to treat cataracts.
- An ophthalmologist is a medical doctor (M.D.) who specializes in the medical and surgical care of the eye.
- An optometrist is a doctor of optometry (O.D.) who practices eye care and prescribes corrective lenses but does not perform surgery.
Diagnostic Tests
The eye professional can observe cloudy areas on the lenses with a physical examination, even before the cataracts begin to interfere with vision. Cameras can measure the cataract density. Various vision tests are also performed.
Snellen Eye Chart. To determine how clearly a person can actually see, the Snellen eye chart is used, with rows of letters decreasing in size:
- From a specified distance, usually 20 feet, a person reads the letters using one eye at a time.
- If a person can read down to the small letters on the line marked 20 feet, then vision is 20/20 (normal vision).
- If a person can read only down through the line marked 40 feet, vision is 20/40; that is, from 20 feet the patient can read what someone with normal vision can read from 40 feet.
- If the large letters on the line marked 200 feet cannot be read with the better eye, even with glasses, the patient is considered legally blind.
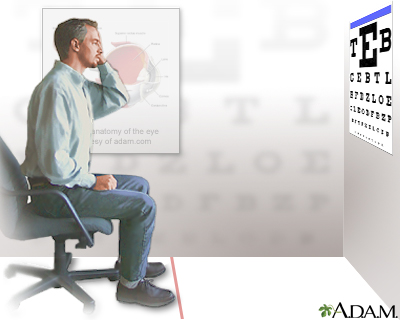
Other Tests. A number of other tests are used to diagnose cataracts or to determine if surgery is needed.
- A chart similar to the Snellen chart, which has the same size letters, but in different contrasts with background, is used to test contrast sensitivity.
- Glare sensitivity is tested by having the patient read a chart twice, with and without bright lights.
- Tests of macular function, which evaluate the eye's acute vision center, can help the ophthalmologist determine the expected improvement from surgery.
- The corneal endothelium, a layer of cells lining the cornea, is sensitive to surgical trauma and should be evaluated before any intraocular operation.
- Patients with other eye disorders may need other pre-operative tests.
Although eye tests help confirm a diagnosis of cataracts, results do not always reflect the quality of life and how effectively people function at home:
- Some people with cataracts perform poorly on the tests yet have no trouble with daily function.
- Others perform well on the tests but find that their eyesight is bad enough to interfere with ordinary activities, such as driving.
Treatment
Although surgery is the only remedy for cataracts, it is almost never an emergency. Most cataracts cause no problem other than reducing a person's ability to see, so there is no harm in delaying surgery.
The following measures may manage early cataracts:
- Stronger eyeglasses or contact lenses
- Use of a magnifying glass during reading
- Strong lighting
- Medication that dilates the pupil. (This may help some people with capsular cataracts, although glare can be a problem with this treatment.)
Progression of Cataracts. Patients and their families usually have plenty of time to carefully consider options and discuss them with an ophthalmologist. There is no constant rate at which cataracts progress:
- Some cataracts develop to a certain point and then stop.
- Even if a cataract does progress, it may be years before it interferes with vision.
- It is very rare for people to need immediate cataract surgery.
Choosing Cataract Surgery
Cataract removal is the one of the most common type of eye surgeries performed in the United States, especially for people over age 65. In the past, cataract surgery was not performed until the cataract had become well developed. Newer techniques, however, have made it safer and even more efficient to operate in earlier stages. Cataract surgery improves vision in up to 95% of patients and prevents millions of Americans from going blind.
Nevertheless, cataract surgery may be performed more often than needed. In general, even if cataracts are diagnosed, the decision to remove them should be based on the patient's own perception of vision difficulties and the effect of vision loss on normal activity. The patient should also be aware of all the risks and costs of surgery.
Indications for Surgery
In general, surgery is indicated for people with cataracts under the following circumstances:
- The Snellen eye test reports 20/40 or worse, with a cataract being responsible for vision loss that cannot be corrected by glasses.
- Performing everyday activities has become difficult to perform to the point that independence is threatened, or the patient is at risk for accident or injury.
These guidelines are general, however. Whether surgery is appropriate or not further depends on the cataract patient's specific condition and needs. Some examples include:
- Even if the criteria for surgery are met, a very sick, elderly person in a nursing home may have less need for sharp vision than an active younger adult. Among very elderly patients (85 years and older), especially those with serious health problems, there are also higher risks for complications during surgery and poorer outcomes afterward. Nevertheless, advanced age alone should not prevent someone from having this procedure.
- Even if the criteria for surgery are not met, some people with eye tests of 20/40 or better might want surgery because of problems with glare, double vision, or the need to have an unrestricted driver's license.
- Even if the criteria for surgery are not met, if retinal disease is also suspected (usually a complication of diabetes), the doctor may perform cataract surgery in order to have a clear view of the eye.
Because of the risks, albeit small ones, of poorer vision or blindness, no one should be forced to have cataract surgery if they don't want it or are not strong enough to have the procedure. If there are any doubts about whether or not to have cataract surgery, consider a second opinion.
Questions for the Ophthalmologist
The patient should ask the ophthalmologist the following questions before agreeing to cataract surgery:
- Is my cataract surgery an emergency?
- Are the cataracts the only cause of my poor vision?
- How much experience do you have with this procedure?
- Do I have other eye diseases that might complicate surgery or reduce my benefit?
- Do I have other health problems that might further complicate eye surgery?
- What type of lens will you implant?
- What type of procedure will you use?
- Afterward, what are my chances of having poorer vision or becoming totally blind in that eye?
- How well should I ultimately be able to see out of the operated eye?
- How long will it take to heal?
- What precautions should I take during the healing process?
- How long will it take to achieve my best eyesight?
- Will I have to wear glasses or contact lenses after surgery?
- When will I get my final eyeglass prescription?
- How soon after surgery will I be able to see well enough to go back to work? Drive a car? Return to full activity?
Treatment for Patients with Accompanying Eye Conditions
Cataracts in the Second Eye. If a person has a cataract in a second eye, the issues for decision making are the same as for the first eye. The best timing for the operation in the case of two cataracts is unclear. Doctors have long recommended postponing surgery on the second eye until the first eye has healed and the results are known. However, many patients have trouble reading and performing ordinary tasks while waiting for a second surgery. Patients with cataracts in both eyes should discuss all options with their eye surgeon.
Cataracts and Glaucoma. For patients with both glaucoma and cataracts, doctors recommend:
- In patients with cataracts and poorly controlled glaucoma, a two-step procedure for both eye conditions may be used. The patient first receives a trabeculectomy for glaucoma, followed by cataract surgery. Fluid leakage and the presence of blood in the back chamber of the eye are potential complications of this combined procedure. Phacoemulsification has improved success rates and reduced high complication rates of the double procedure compared with extracapsular cataract extraction. New advances that replace trabeculectomy with nonpenetrating glaucoma surgery may prove to be beneficial.
- In patients who have cataracts plus either closed-angle glaucoma or open angle glaucoma that is stabilized with medication, the cataract may be extracted and medication continued for the glaucoma.
Cataracts and Corneal Disease. Patients with both cataracts and corneal disease may have one of the following procedures:
- Combination Procedure. A single operation that combines three procedures, extracapsular cataract extraction and intraocular lens insertion with corneal transplantation (called penetrating keratoplasty).
- Sequential Procedure. An operation that uses two procedures sequentially. The sequential option performs the cataract procedures and the corneal transplantation separately.
Treating Cataracts in Children
Infants. Treatment of infants first depends on whether one or both eyes are affected:
- For infants born with cataracts in one eye, the American Academy of Ophthalmology recommends surgery as soon as possible, by age 4 months or ideally even earlier. The procedure is followed by contact lens correction and patching of the unaffected eye. Although this approach is successful in many cases, some children still become blind in the affected eye. There is also a high risk for glaucoma after surgery.
- In infants with cataracts in both eyes, surgery is not always an option. Sometimes surgery may be performed sequentially, with the second eye operated on a few days after the first. Phacoemulsification appears to pose a much higher risk for secondary cataracts than standard lens removal.
Toddlers and Older Children. Intraocular lens replacement is now standard treatment for children age 2 years and older.
Surgery
Preparing for Cataract Surgery
Cataract surgery is usually done as an outpatient procedure under local anesthesia and takes less than an hour. Preoperative preparations may include:
- Having a general physical examination is important for patients with medical problems such as diabetes. Diabetes can cause damage to the blood vessels of the eye’s retina, a condition called diabetic retinopathy. Research suggests that patients who have diabetic retinopathy and poor blood sugar control should not have their blood sugar rapidly corrected before cataract surgery. Correcting blood sugar too quickly before surgery may cause vision problems after surgery.
- Reviewing all medications with the ophthalmologist. In particular, men who take tamsulosin (Flomax, generic), or similar drugs for prostate problems, require special surgical techniques to prevent complications.
- The ophthalmologist will use a painless ultrasound test to measure the length of the eye and determine the type of replacement lens that will be needed after the operation.
- Topical antibiotics (such as ofloxacin or ciprofloxacin) may be applied preoperatively to protect against postoperative infection.
- Most healthy patients receive either a local injection or topical anesthetic. They may also receive a sedative. Some patients may need general anesthesia.
Surgical Procedures
All cataract procedures involve removal of the cataract-affected lens and replacing it with an artificial lens.
Phacoemulsification. Phacoemulsification (phaco means lens; emulsification means to liquefy) is the most common cataract procedure performed in the United States.
The procedure generally involves:
- The surgeon makes a small incision.
- A thin probe that transmits ultrasound is used to break up the clouded lens into small fragments.
- The tiny pieces are sucked out with a vacuum-like device.
- A replacement lens is then inserted into the capsular bag where the natural lens used to be. In most cases, this is an intraocular lens (IOL), which is foldable and slips in through the tiny incision.
- Because the incision is so small, it is often watertight and does not require a suture afterward, particularly if a foldable lens has been used. A suture may be needed if a tear or break occurs during the procedure or the surgeon inserts a rigid lens that requires a wider incision.
Phacoemulsification requires only local anesthesia. Most phacoemulsification procedures take about 15 minutes, and the patient is usually out of the operating room in about an hour. There is little discomfort afterward, and visual rehabilitation takes about 1 - 3 weeks.
Phacoemulsification is sometimes combined with glaucoma surgical procedures, for patients who have both glaucoma and cataracts.
Extracapsular or Intracapsular Cataract Extraction. Extracapsular cataract extraction, the original standard procedure, is now generally used only in patients who have an extremely hard lens. It typically involves the following steps:
- The surgeon works under an operating microscope to make a small incision in the cornea of the eye.
- The surgeon extracts the clouded lens through this incision.
- The capsule is left in place, which adds structural strength to the eye and enhances the healing process. (Less commonly in intracapsular cataract extraction, the surgeon removes the lens and the entire capsule. This procedure has greater risks for swelling and retinal detachment.)
- A replacement lens is then usually inserted.
- A small suture is needed to stitch the incision together.
It takes about 2 - 4 weeks for vision to be completely restored.
Replacement Lenses and Glasses
With the clouded lens removed, the eye cannot focus a sharp image on the retina. A replacement lens or eyeglasses are therefore needed:
Intraocular Lenses (IOLs). In about 90% of cataract operations, an artificial lens, known as an intraocular lens (IOLs), is inserted. Most IOLs are made out of acrylic, although other materials, such as silicon, are also used.
IOLs are designed to improve specific aspects of vision. The choices include:
- Lenses that address a single fixed focal point. Such lenses are suitable either for reading or distance vision, but not both. If a distance lens is implanted, the surgeon prescribes glasses or contact lenses for reading. If a reading lens is implanted, lenses for seeing distances will be prescribed.
- Lenses that address multifocal points. Multifocal lenses can focus at different points for both reading and distance vision. However, contrast may be reduced, and some patients experience glare and halos, particularly at night.
- Lenses are available to correct astigmatism after cataract surgery.
The patients and the doctor must make these decisions based on specific visual needs. Many patients also need eyeglasses after cataract surgery for reading or to correct astigmatism.
Complications of Cataract Surgery
Cataract surgery is one of the safest of all surgical procedures. Most complications, even if they occur, are not serious. They can include:
- Swelling and inflammation can occur in the days or weeks following surgery. Risk is about 1%. This complication can be particularly harmful for patients with existing uveitis (chronic inflammation in the eye, which can be due to various medical conditions).
- Retinal detachment. In rare cases, the retina at the rear of the eye can become detached.
- Glaucoma. This is an eye condition in which the pressure of fluids inside the eye rises dangerously. Risk is very low, but patients should be sure to avoid activities after surgery that increase pressure.
- Infection. This is very rare (0.2%) but may be significant if it does develop.
- Bleeding can develop inside the eye.
- Posterior capsular opacification is one the more common complications of cataract surgery. The risk appears to be lower with sharp-edged (square) IOLS than round IOLs.
Preventing Infection and Reducing Swelling. The ophthalmologist may prescribe the following medications after surgery:
- A topical antibiotic may protect against infection.
- Corticosteroid eyedrops or ointments are often used to reduce swelling, but they can pose a risk for increased pressure in the eye.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as diclofenac, ketorolac, naproxen, and voltaren, also reduce swelling and do not have the same risks as steroids. Newer NSAIDs approved to treat pain and swelling after cataract surgery include bromfenac (Xibrom) and nepafenac (Nevanac).
Factors that Increase Risk for Complications. The risks of complications are greater for the following people:
- Patients who have other eye diseases.
- People with diabetes. Intracapsular and extracapsular cataract extraction can pose a high risk for the development or worsening of retinopathy, a known eye complication of diabetes.
- People who have taken tamsulosin (Flomax, generic) or other alpha-1 blocker drugs. Tamsulosin is a muscle relaxant prescribed for treatment of several urinary conditions, including benign prostatic hyperplasia (BPH). Tamsulosin may cause intraoperative floppy iris syndrome (IFIS), a loss of muscle tone in the iris that can cause complications during eye surgery. Problems have been reported both for patients who were taking the drug during surgery as well as those who had stopped taking the drug weeks or months before surgery. Men who have taken tamsulosin or similar drugs should inform their eye surgeon. The surgeon may need to use different techniques to minimize the risk of IFIS and other complications.
Postoperative Care
Returning Home and Follow-up Visits.
- Patients usually leave the surgical site within an hour of surgery. Cataract surgery almost never requires an overnight hospital stay.
- Patients need someone to drive them home and stay with them for a few days until their vision improves.
- The patient is usually examined the day after surgery and then during the following month. Additional visits occur as necessary.
- Vision usually remains blurred for a while but gradually clears, usually over 2 - 6 weeks. (It can take longer.)
- When the doctor decides the condition has stabilized, the patient will receive a final prescription for glasses or contacts.
Protecting the Eye. Postoperative protection of the eye typically involves:
- The ophthalmologist usually tapes a bandage over the eye to protect it during the healing process.
- When changing the bandage, the eye can be cleaned gently using a washcloth dipped in warm water without soap. A new bandage can then be positioned and taped.
- It is very important not to press or rub the eye during this procedure.
- An eye shield may be placed over the bandage at night.
Avoiding Glaucoma. Cataract surgery can cause glaucoma, a condition in which the pressure of fluids inside the eye rises dangerously. It is very important to minimize any activity that increases internal eye pressure. Postoperative cataract patients should take the following precautions:
- Minimize vigorous exercise.
- Put on shoes while sitting and without bending over.
- Kneel instead of bending over to pick something up.
- Avoid lifting.
- Limit reading since it requires eye movement (watching television is all right).
- Sleep on the back or on the unoperated side.
Treatment of Posterior Capsular Opacification (Secondary “After Cataract”)
About 15% of patients who have cataract surgery develop a secondary "after-cataract" called posterior capsular opacification. Posterior capsular opacification is a clouding of the lens capsule that was left behind when the original cataract was removed. It generally occurs because after surgery there are still some natural lens cells left behind that proliferate on the back of the capsule.
The standard treatment for posterior capsular opacification is a type of laser surgery known as a YAG capsulotomy. (Capsulotomy means cutting into the capsule, and YAG is an abbreviation of yttrium aluminum garnet, the laser most often used for this procedure.) This procedure can help improve vision and reduce glare.
- This is an outpatient procedure and involves no incision.
- Using the laser beam, the ophthalmologist makes an opening in the clouded capsule to let light through.
- After the procedure, the patient remains in the doctor's office for an hour to make sure that pressure in the eye is not elevated.
- The doctor will usually prescribe anti-inflammatory eyedrops for the patient to take at home.
- Most patients will find that their vision improves within a day.
- An eye examination for any complications should follow within 2 weeks.
Complications. YAG laser capsulotomy is generally a safe procedure. Serious complications are rare, but can include retinal detachment.
Resources
- www.ascrs.org -- The American Society of Cataract and Refractive Surgery
- www.aao.org -- American Academy of Ophthalmology
- www.nei.nih.gov -- National Eye Institute
- www.eyesurgeryeducation.org -- Eye Surgery Education Council
- www.lighthouse.org -- Lighthouse International
- www.aao.org/aao/find_eyemd.cfm -- Find an ophthalmologist
References
American Academy of Ophthalmology. Cataract in the Adult Eye, Preferred Practice Pattern. San Francisco: American Academy of Ophthalmology, 2006. Accessed July 1, 2008.
Awasthi N, Guo S, Wagner BJ. Posterior capsular opacification: a problem reduced but not yet eradicated. Arch Ophthalmol. 2009 Apr;127(4):555-62.
Bell CM, Hatch WV, Fischer HD, Cernat G, Paterson JM, Gruneir A, et al. Association between tamsulosin and serious ophthalmic adverse events in older men following cataract surgery. JAMA. 2009 May 20;301(19):1991-6.
Christen WG, Glynn RJ, Sesso HD, Kurth T, MacFadyen J, Bubes V, et al. Age-related cataract in a randomized trial of vitamins E and C in men. Arch Ophthalmol. 2010 Nov;128(11):1397-405.
Clinical Trial of Nutritional Supplements and Age-Related Cataract Study Group, Maraini G, Sperduto RD, Ferris F, Clemons TE, Rosmini F, et al. A randomized, double-masked, placebo-controlled clinical trial of multivitamin supplementation for age-related lens opacities. Clinical trial of nutritional supplements and age-related cataract report no. 3. Ophthalmology. 2008 Apr;115(4):599-607.e1.
Fernandez MM, Afshari NA. Nutrition and the prevention of cataracts. Curr Opin Ophthalmol. 2008 Jan;19(1):66-70.
Findl O, Buehl W, Bauer P, Sycha T. Interventions for preventing posterior capsule opacification. Cochrane Database Syst Rev. 2010 Feb 17;2:CD003738.
Friedman AH. Tamsulosin and the intraoperative floppy iris syndrome. JAMA. 2009 May 20;301(19):2044-5.
Guercio JR, Martyn LJ. Congenital malformations of the eye and orbit. Otolaryngol Clin North Am. 2007 Feb;40(1):113-40, vii.
Moeller SM, Voland R, Tinker L, Blodi BA, Klein ML, Gehrs KM, et al. Associations between age-related nuclear cataract and lutein and zeaxanthin in the diet and serum in the Carotenoids in the Age-Related Eye Disease Study, an Ancillary Study of the Women's Health Initiative. Arch Ophthalmol. 2008 Mar;126(3):354-64.
Olitsky SE, Hug D, Plummer LS, and Stass-Isern M. Abnormalities of the lens. In: Kliegman RM, Stanton BF, St. Geme III JW, Schor NF, Behrman RE, eds. Nelson Textbook of Pediatrics. 19th ed. St. Louis, MO: WB Saunders; 2011; chap 620.
Vizzeri G, Weinreb RN. Cataract surgery and glaucoma. Curr Opin Ophthalmol. 2010 Jan;21(1):20-4.
|
Review Date:
9/10/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M. Health Solutions, Ebix, Inc. |









